Understanding Cluster Headache
Cluster headache is a rare but extremely painful type of headache that affects about 0.1% of the population. Known for being one of the most excruciating forms of pain, cluster headache can significantly impact the quality of life.
This guide provides an overview of cluster headache, their symptoms, treatment options, and guidance on when to see a healthcare provider.
What is a Cluster Headache?
Cluster headache is characterized by intense, recurring pain on one side of the head, often around or behind the eye. The pain is typically described as a 10 out of 10 on the pain scale and can be more severe than labor pain, gunshot wounds, or heart attack pain.
- Location of Pain: Strictly unilateral (one-sided), but can alternate sides in some people, with pain that occurs around or behind the eye, forehead, and temple.
- Pain Severity: Severely painful and described as feeling an ice pick or hot poker drive through the eye or temple. The pain strikes suddenly and reaches its peak within 3 to 5 minutes.
- Duration: Attacks last between 15 minutes to 180 minutes (3 hours), occurring several times a day (1-8 times).
- Symptoms: May include at least one of the following: tearing of the eye, nasal congestion, drooping eyelid, constriction of the pupil on the affected side, and forehead and facial sweating, may also include a sense of restlessness or agitation.
- Types: Cluster headache exists in two types: episodic or chronic. Approximately 80% of individuals with cluster headache are episodic. Attacks only occur during a period of weeks to months, with attack-free periods. The remainder are chronic, with attacks occurring around the same time of the day or regularly without significant attack-free periods longer than 3 months. An estimate of 15% of patients may also transition from one type to another. [1]
- Sex Prevalence: In a conducted survey of 1,604 individuals with cluster headache, 68.8% were male, and 31.0% were female. Female respondents were more likely to have chronic cluster headache and reported experiencing higher pain intensity compared to males. They also had higher depression scores, more frequent nausea and vomiting, and greater aggravation of symptoms with physical movement. [2] These findings, in part, reflect a misdiagnosis in women, where cluster headache is sometimes mistaken for migraine. [3]
Common Triggers for Cluster Headache
- Smoking: Tobacco use and its causation for cluster headache are unclear. However, tobacco exposure could be a risk factor, increasing the frequency of an attack and the cycle duration. [4]
- Alcohol: Alcohol consumption can trigger cluster headache attacks in 40-80% of individuals. [5]
- Regular Timing: Attacks often occur with clock-like regularity, sometimes waking up individuals at the same time each night.
- Environmental: High altitude (air travel, mountain climbing), weather conditions (temperature, barometric pressure changes), and intense sunlight can trigger attacks. [6]
Treatment Options for Cluster Headache
Preventative Treatments
- Prednisone: A steroid used in tapering doses for about 10-14 days, usually serving as a bridge that allows another preventative drug to begin working – timing and dosing to be determined by your healthcare provider. ACTH (adrenocorticotropic hormone) may also be considered afterwards by your healthcare provider.
- Verapamil: A calcium channel blocker that is often used at higher doses (240-480 mg/day, usually taken in divided doses). Dosage should be carefully monitored due to potential heart-related side effects.
- Galcanezumab: A CGRP monoclonal antibody specifically approved for episodic cluster headache.
- Neuromodulator gammaCore™ (non-invasive vagus nerve stimulator [nVNS]) is FDA cleared for the adjunctive use for the preventive treatment of cluster headache in adult patients.
Acute Treatments
- Oxygen Therapy: Inhalation of high-flow oxygen (10-15 liters per minute) through a non-rebreather mask can provide rapid relief. Some individuals may find additional benefit from using a mask specifically designed for people living with cluster headache. Learn more about this type of mask.
Disclaimer: This resource is provided for informational purposes only and does not represent an endorsement of any specific product or brand by the National Headache Foundation.
- Triptans: Fast-acting formulations, such as sumatriptan injections or nasal sprays, can be effective in treating acute cluster attacks.
- DHE (dihydroergotamine): Ask your healthcare provider whether this option might be right for you.
- Neuromodulator gammaCore™ (non-invasive vagus nerve stimulator [nVNS]) is FDA cleared for the adjunctive use for the preventive treatment of cluster headache in adult patients.
When to Talk With a Healthcare Provider
You should consult a healthcare provider if you:
- Experience severe, sudden-onset headache attacks that are among the worst pain you have ever felt.
- Have headache attacks that occur in a cyclical pattern or at the same time each day.
- Notice symptoms like tearing, nasal congestion, or drooping of the eyelid on the affected side.
- Suspect you have cluster headache and have not yet received a proper diagnosis or treatment plan.
A headache specialist or neurologist can help diagnose cluster headache and provide tailored treatment options. Individuals experiencing cluster headache symptoms should receive an MRI to help rule out other serious or life-threatening conditions.
Cluster headache is an incredibly painful and debilitating condition that requires prompt medical attention and tailored treatment. Understanding the symptoms and triggers can help manage the condition effectively. If you suspect you have cluster headache, consult a healthcare provider to explore preventive and acute treatment options that best suit your needs.
Finding Community
If you or a loved one is living with cluster headache, know that you’re not alone. While the information on this page offers a starting point for understanding symptoms and treatments, additional support and advocacy resources are available.
We encourage you to visit Clusterbusters, a leading organization dedicated specifically to people with cluster headache. Their work includes patient education, research, advocacy, and community-building.
Learn More
Learn More Through Personal Stories

Bob’s journey with cluster headache began in his mid-20s, when the condition dramatically changed the course of his life. Over the next two decades, he tried an astounding 70 different medications and hundreds of combinations, with little relief.
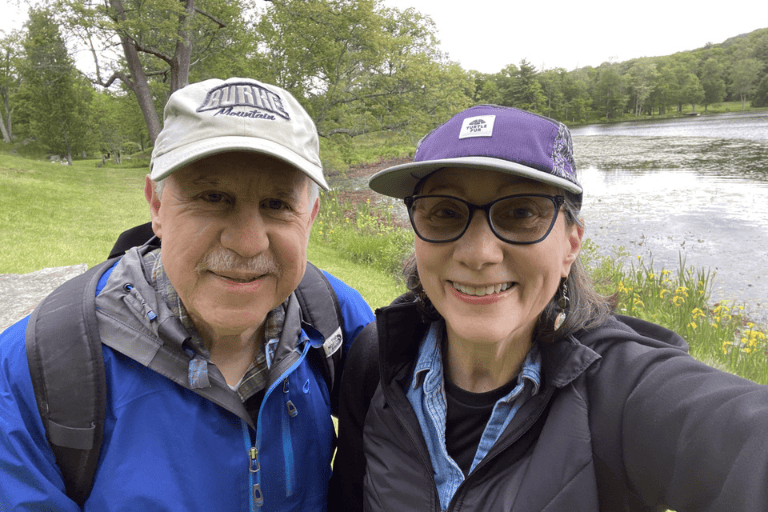
Now in his late 60s and living in Woodstock, New York, the retired environmental planner reflects on his challenging journey of battling cluster headache for several decades, a condition that disrupted work, family life, and even moments of mourning.

Ashley’s journey with cluster headache began at just 18 years old, right as she was starting college. What started as brief, stabbing pains in her head quickly morphed into debilitating cluster headache attacks that would last for hours at a time.
References
[1] Schindler, E. A. D., & Burish, M. J. (2022). Recent advances in the diagnosis and management of cluster headache [PDF]. https://www.binasss.sa.cr/bibliotecas/bhm/abr/3.pdf
[2] Schor, L. I., Pearson, S. M., Shapiro, R. E., Zhang, W., Miao, H., & Burish, M. J. (2021). Cluster headache epidemiology including pediatric onset, sex, and ICHD criteria: Results from the International Cluster Headache Questionnaire. Headache: The Journal of Head and Face Pain, 61(10), 1511-1520. https://doi.org/10.1111/head.14237
[3] San-Juan, D., Velez-Jimenez, K., Hoffmann, J., Martínez-Mayorga, A. P., Melo-Carrillo, A., Rodríguez-Leyva, I., García, S., Collado-Ortiz, M. Á., Chiquete, E., Gudiño-Castelazo, M., Juárez-Jimenez, H., Martínez-Gurrola, M., Marfil, A., Nader-Kawachi, J. A., Uribe-Jaimes, P. D., Darío-Vargas, R., & Villareal-Careaga, J. (2024). Cluster headache: an update on clinical features, epidemiology, pathophysiology, diagnosis, and treatment. Frontiers in pain research (Lausanne, Switzerland), 5, 1373528. https://doi.org/10.3389/fpain.2024.1373528
[4] Rozen T. D. (2018). Cluster Headache Clinical Phenotypes: Tobacco Nonexposed (Never Smoker and No Parental Secondary Smoke Exposure as a Child) versus Tobacco-Exposed: Results from the United States Cluster Headache Survey. Headache, 58(5), 688–699. https://doi.org/10.1111/head.13295
[5] Schindler, E. A. D., & Burish, M. J. (2022). Recent advances in the diagnosis and management of cluster headache [PDF]. https://www.binasss.sa.cr/bibliotecas/bhm/abr/3.pdf
[6] Schindler, E. A. D., & Burish, M. J. (2022). Recent advances in the diagnosis and management of cluster headache [PDF]. https://www.binasss.sa.cr/bibliotecas/bhm/abr/3.pdf
Subscribe for News and Updates
Stay informed with the latest news, updates, and episodes from the HeadWise podcast.