STRENGTH IN EVERY STORY™
Penny’s Story, November 2024
As told by: Valerie Stevens, Edited by Fabiola Palomo
Diagnosis received: Chronic daily migraine
Symptoms: Daily head pain, Sensitivity to barometric pressure changes
As a nurse, Penny has spent her career caring for others but for years, she’s also been quietly struggling with a condition of her own. Migraine has been a constant, unwelcome companion in Penny’s life. Her journey began around age 12, coinciding with her menstrual cycle with attacks that struck with a crushing intensity.
 “Every month my head felt like it would explode,” she recalled. Back then, 1- 2 days of pain each month didn’t seem uncommon, and the way to find relief was by taking an over-the-counter pain reliever such as acetaminophen, aspirin, and caffeine to help manage her symptoms.
By the time Penny was 25 and navigating a divorce, the migraine attacks had grown more frequent. A visit to her first neurologist resulted in getting a prescription for nortriptyline, but it brought more side effects than relief.
She stopped the medication soon after, choosing instead to simply hope for the best and move forward with life. “The migraines continued, but I went on and lived my life the best I could.”
In her 30s, as a single mother working part-time, Penny attributed the attacks to stress. Over-the-counter medications were the only interventions she found to better manage her symptoms. Then came her 40s and a new level of emotional strain. Her sister, best friend, and anchor in life was diagnosed with Stage 4 cancer. As a nurse, Penny suspected she was terminal. “That was [a] real stress! I was her primary caregiver; she and her husband were not on the best terms [and] 7 months after her diagnosis, she passed away.”
“Every month my head felt like it would explode,” she recalled. Back then, 1- 2 days of pain each month didn’t seem uncommon, and the way to find relief was by taking an over-the-counter pain reliever such as acetaminophen, aspirin, and caffeine to help manage her symptoms.
By the time Penny was 25 and navigating a divorce, the migraine attacks had grown more frequent. A visit to her first neurologist resulted in getting a prescription for nortriptyline, but it brought more side effects than relief.
She stopped the medication soon after, choosing instead to simply hope for the best and move forward with life. “The migraines continued, but I went on and lived my life the best I could.”
In her 30s, as a single mother working part-time, Penny attributed the attacks to stress. Over-the-counter medications were the only interventions she found to better manage her symptoms. Then came her 40s and a new level of emotional strain. Her sister, best friend, and anchor in life was diagnosed with Stage 4 cancer. As a nurse, Penny suspected she was terminal. “That was [a] real stress! I was her primary caregiver; she and her husband were not on the best terms [and] 7 months after her diagnosis, she passed away.” 
One day after work, alone in her room, she felt her sister’s presence. A message came through clearly and became a turning point for Penny’s life. “‘Stop feeling sad and do something.’”
Being a nurse and certified exercise instructor, she began channeling her grief into purpose and started a nonprofit organization offering support to cancer patients and their loved ones. “Yoga classes were our first offering. The organization grew rapidly; other programs and support groups were [later] introduced [as well].”
But with every step forward came new stress. Juggling her nonprofit, raising her daughter, and working full-time, Penny threw herself into a mission, yet remained resilient. “The headaches got worse, but I persevered, I was obsessed with my new concept in life,” shared Penny.
When her sister’s oncologist invited her to join his practice, she accepted, adding yet another role to her already full plate. “Was I crazy? Volunteering for a new non-profit 24/7, now placing a new job in the mix, I must be crazy!”
Due to this, the attacks worsened and became daily, with only temporary relief. “Working a stressful job, running an organization pretty much by myself, the headaches became daily. I tried abortives* [and] they helped temporarily but returned with a vengeance.”
Eventually, Penny made the once difficult but necessary choice to prioritize her own health. “I finally gave in and made the time to seek out a new neurologist. [Asking herself,] ‘How could I help others when I wasn’t taking care of myself?’”
The neurologist ordered an MRI, which revealed “white matter” on her brain—a result of the constant headache attacks. Despite a new treatment plan that included medications and multiple rounds of onabotulinumtoxinA [injections], nothing worked. When her healthcare provider relocated, she was referred to a headache center. There, doctors tried different treatment combinations, including inpatient care at a local hospital. Still, the pain persisted.

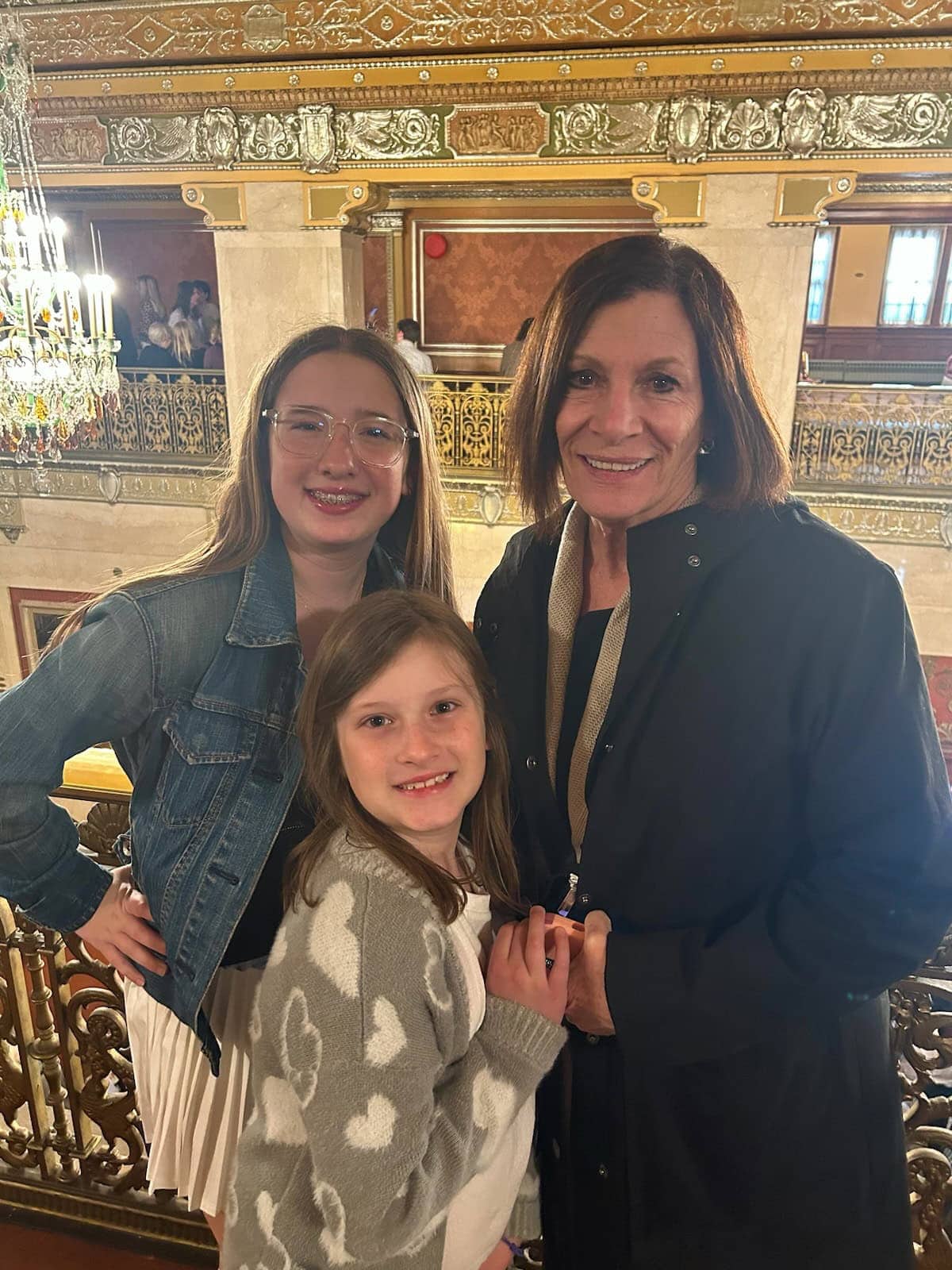
Meanwhile, life continued. Penny’s daughter grew up, married, and was expecting her second child in Pittsburgh. Determined not to miss out on being a part of her grandchildren’s lives, Penny and her husband packed up and moved five hours away from home and everything they knew.
Hope came in the form of a respected neurologist affiliated with a major teaching hospital in Pittsburgh. She placed Penny on topiramate, increasing the dosage when initial results were ineffective. Instead of getting relief, Penny’s cognition began to decline. Her husband noticed it first with signs of depression. “All it did was concern my family that at the young age of 60, I had dementia or Alzheimer’s,” said Penny.
She was eventually referred to a neuropsychologist for four hours of cognitive testing. The results confirmed it wasn’t dementia, but the medication. She immediately began weaning off the topiramate, “I felt like a whole new person…[but] my headaches were still there.”
Back she went to a headache center, once again facing inpatient care, but nothing made a lasting difference. Healthcare providers reassured her that as she aged, the attacks might lessen over time. She tried nearly everything. The newer class of medications, CGRPs, offered hope, but each one failed. In a final effort, she endured a five-day hospital stay for ketamine therapy. When that didn’t work, her headache specialist referred her to an oral surgeon specializing in onabotulinumtoxinA treatments. Though skeptical, Penny agreed to give it another try.
After the third round, some relief came. “The headaches were not as intense [as] I started having a few headache-free days.” Seeing that the injection treatment provided some relief, she tried the treatment for a year, only to be met with hardship again as it lost its effectiveness.
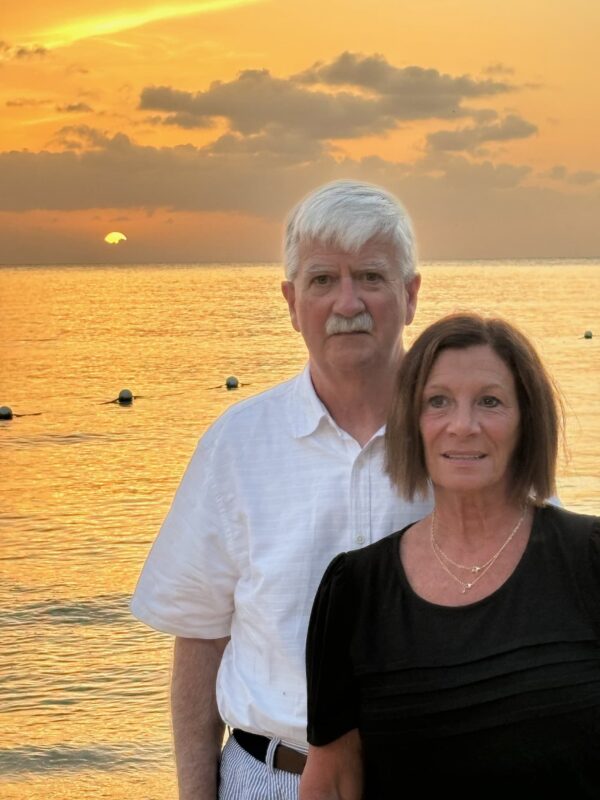
Today, Penny still wakes up each morning with a headache, with pain levels ranging from 4 to 20. Rimegepant, taken every other day, provides some short-term relief. However, most treatments have offered little or no lasting help. While the pain never completely leaves, she considers herself lucky for having her family be the greatest support system.
Now, there’s a new direction for Penny as she’s found out she qualifies for a clinical trial at a headache center that involves implanting a neurostimulator on each side of her head for a year. “I’m not thrilled about having this, but I failed every other treatment,” admitted Penny.
At 70 years old and still working part-time, Penny can’t picture stepping away from the career that has shaped so much of her life, “I can’t see myself not being a nurse anymore!”
Still, the physical and emotional toll of migraine is real. “Living in chronic pain exhausts one’s mental and physical being,” Penny shared. “Some days it takes all my mental strength to go to work or stay off the couch in a fetal position. My headache specialist calls me a warrior! I don’t know about that but working with dying or seriously ill people puts my life in perspective.”
After years of working in oncology and hospice, Penny holds a grounded perspective. “I don’t fool myself into thinking I’ll die from these headaches, it’s just an inconvenience.”
Still, she knows the toll migraine and headache disorders take on those who suffer in silence—and hopes that by sharing her story, others will feel seen, heard, and less alone.
Penny’s story is a powerful reminder that even those who work within the healthcare system can find it incredibly difficult to navigate when seeking care for themselves. As a nurse, Penny brought both medical knowledge and advocacy skills to her own journey yet faced years of ineffective treatments and persistent pain. Her experience reflects the real and authentic challenges individuals with migraine face, especially when standard options fall short.
While there is no easy resolution, Penny’s story gives voice to a community often overlooked and illustrates the urgent need for continued research, understanding, and access to comprehensive, compassionate care.
*Abortive migraine medications are used to relieve the symptoms of a migraine attack as it is occurring.
"*" indicates required fields
