STRENGTH IN EVERY STORY™
Kate’s Story, March 2025
As told by: Fabiola Palomo
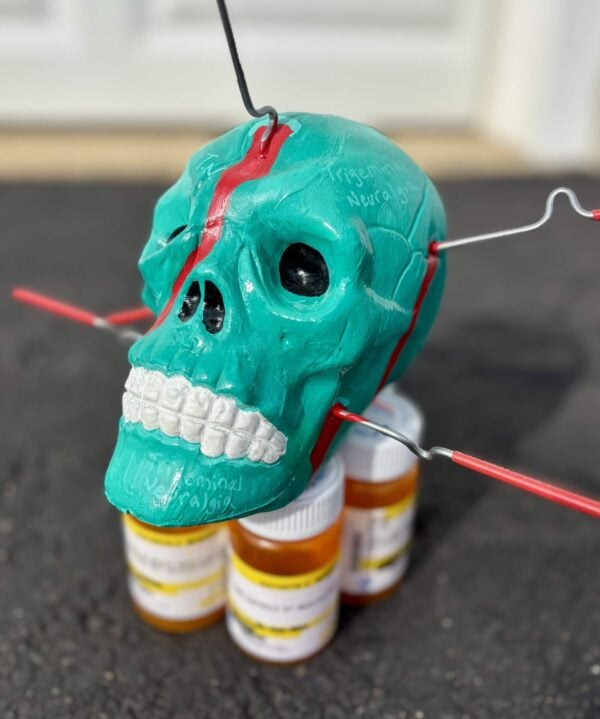
Diagnosis received: Trigeminal neuralgia, Chronic Migraine
Symptoms: Nausea, Sensitivity to wind, Sensitivity to light, Sensitivity to sound, Visual disturbances
Kate, a U.S. Coast Guard veteran, who served for 13 years, was occasionally stationed in radiation fallout areas, including Kodiak, Alaska, where she suspects her thyroid tumor developed. Discovering it was cancerous, Kate underwent surgery to remove it. Complications during the procedure injured her cervical spine, leading to trigeminal neuralgia, a condition in which intense shock-like facial pain occurs on one side of the face. In rare cases, like Kate’s, the disease can occur bilaterally, affecting both sides.
Shortly after surgery, Kate would experience excruciating head pain that would later be defined and diagnosed as chronic migraine and trigeminal neuralgia.
Root Causes

Kate remembers the pain she felt after the surgery all too well. “It was [a] pain, unlike what I had ever felt [before]. I felt like I had glass in my throat… I needed something to explode out of my head for the pain to stop, and those two feelings… They never went away,” recalled Kate.
It is rather unknown to Kate why she began experiencing migraine attacks, but she looked for possible causes. “There were about a million times that I hit my head in service, and nothing happened. When I woke up from that surgery, it all just hit me,” said Kate.
It took her nearly 2 years to get her diagnoses: chronic migraine and trigeminal neuralgia after visiting several doctors. “We were mixing opioids*. We were doing all kinds of crazy stuff. Opioids really didn’t work for me. The military just wanted me functioning in some way from 9:00 am to 5:00 pm. They didn’t want me complaining about pain,” admitted Kate, “That was their fix, but I didn’t feel like I was in my own skin.”
Approaching Night and Day Disruptions and Isolation

During service, Kate was an unyielding, high-performing woman. “[During] ‘chow time,’ or meals time, I sat under a 76-caliber weapon, [the] noise… Nothing bothered me,” expressed Kate. This quickly took a turn, as she now describes herself as a “hermit.” “I don’t want to go outside because the wind bothers my trigeminal neuralgia. Loud noises and lights just make [my] migraines worse,” revealed Kate.
Throughout her journey, the circumstances affected Kate’s relationships, as they struggled to comprehend the effects of what it’s like to live with chronic migraine. “My 16-year marriage has ended. I’ve lost most of my military friends. They just don’t have [the] time for somebody that’s in pain all the time,” shared Kate.
To Kate, it’s been challenging having to adjust to life’s changes and the reality she lives in now. “It’s been [an] eye-opening [experience] to go from [being] one human to a totally different human. Everything in my life has changed.”
On a Journey Toward Self-Acceptance

Despite these unforeseen circumstances, she gradually began to reconnect with her resilient spirit. “I had to kill ‘Kate 1.0’ and accept ‘Kate 2.0’, and that took a while. [It became possible with] a lot of therapy and the only way I can lean into [the change is] …trying to get my feet up under me and like Kate 2.0 [through] advocacy [and] standing up for people.”
Through her advocacy, she has instilled and promoted a positive change both in her life and in others facing similar challenges.
Through re-evaluation and changing her perspective on the concept of pain, Kate was allowed to adapt to a new lifestyle.
“What I learned in my previous life was ‘pain is weakness,’ leaving the body. Bleed it out, puke, and rally. Let’s keep moving. So, I had to learn pacing and had to gain a whole new toolbox of ways to take care of myself through guided meditation [and trying] calming [effective] things… that don’t involve medication because I wanted to go a more natural way [of seeking treatment].”
 In the past, Kate often indulged in going to a [shooting] range to get the frustration out of her system. Now, she practices more calming and therapeutic techniques. “Now, when I have high anxiety [and] high pain, I sit down and color or I use one of these new tools that I have—to try and accept me, accept this new pain and lean into what it is that I have. With that, I can help other people. I do teach creative arts for people [that are living] in pain… through the U.S. Pain Foundation.”
In the past, Kate often indulged in going to a [shooting] range to get the frustration out of her system. Now, she practices more calming and therapeutic techniques. “Now, when I have high anxiety [and] high pain, I sit down and color or I use one of these new tools that I have—to try and accept me, accept this new pain and lean into what it is that I have. With that, I can help other people. I do teach creative arts for people [that are living] in pain… through the U.S. Pain Foundation.” Dismissed and Disregarded
When seeking medical attention, Kate recalled her concerns were dismissed and disregarded. “Once I got out, it was kind of a culture shock. The first time I went into an ER, I was a ‘hysterical woman and pain seeking,’ That caught me off guard [and] I left that ER rather frustrated,” lamented Kate.
Later at another emergency room, instead of finding a healthcare provider that understood, she was met with the following: “[The HCP] told me that I had changed so much since I left the military. I probably have migraines because ‘I’m fat now.’ I hadn’t experienced it before in the military because they just want to put us back out on the frontline as quick as they can…now that I’m out [of the military], I see how different sexes, different races…we’re all treated differently. It’s insane!’”
Gaining a New Perspective by Experiencing the Pain of Migraine
Once retired from the military, Kate has been looking into ways to manage her symptoms, including cannabis**. “It’s given me the mobility to leave the house and the ability to think more clearly and be a part of all these things,” said Kate.

Before Kate developed chronic migraine, she was unable to fully comprehend physical pain before experiencing it herself. “Before I had migraines, I did not understand chronic pain at all, and I was unsympathetic to it. So, I do wish we had more sympathy… this… [isn’t] a little headache,” she said.

Now, she has the ability to understand and share the feelings of others with invisible disabilities like chronic migraine, “It affects your whole life. You’re trying different medications. Your body gets used to them. You’re upping doses [and] you’re trying different things. It’s kind of wreaking havoc with your situation, with your body, with your life [and] it does a lot more [damage]… people are thinking, ‘Oh, I’ve had a headache before.’ No, chronic pain is a total life 180. Chronic pain becomes a profound commitment to enduring both discomfort and extreme pain. It is a complex experience that [not only] involves physical pain, [but affects] emotional, and psychological aspects of one’s life.”
*Disclaimer: The use of opioids is not recommended for the treatment of headache disorders or migraine disease. Evidence suggests they may be ineffective and carry significant risks of medication overuse headache and dependance. (American Headache Society, 2019)
**Disclaimer: The use of cannabis is not currently approved by the U.S. Food and Drug Administration for the treatment of headache disorders or migraine disease. While emerging research and patient reports suggest a reduction in migraine frequency and reduced medication intake, the effectiveness and safety of cannabis for migraine management require further scientific investigation. Additionally, cannabis laws and accessibility vary significantly by state, and its use remains regulated under federal law. Individuals should consult with a healthcare provider and review local regulations before considering cannabis as a treatment option. (Practical Neurology, 2021)
"*" indicates required fields
