STRENGTH IN EVERY STORY™
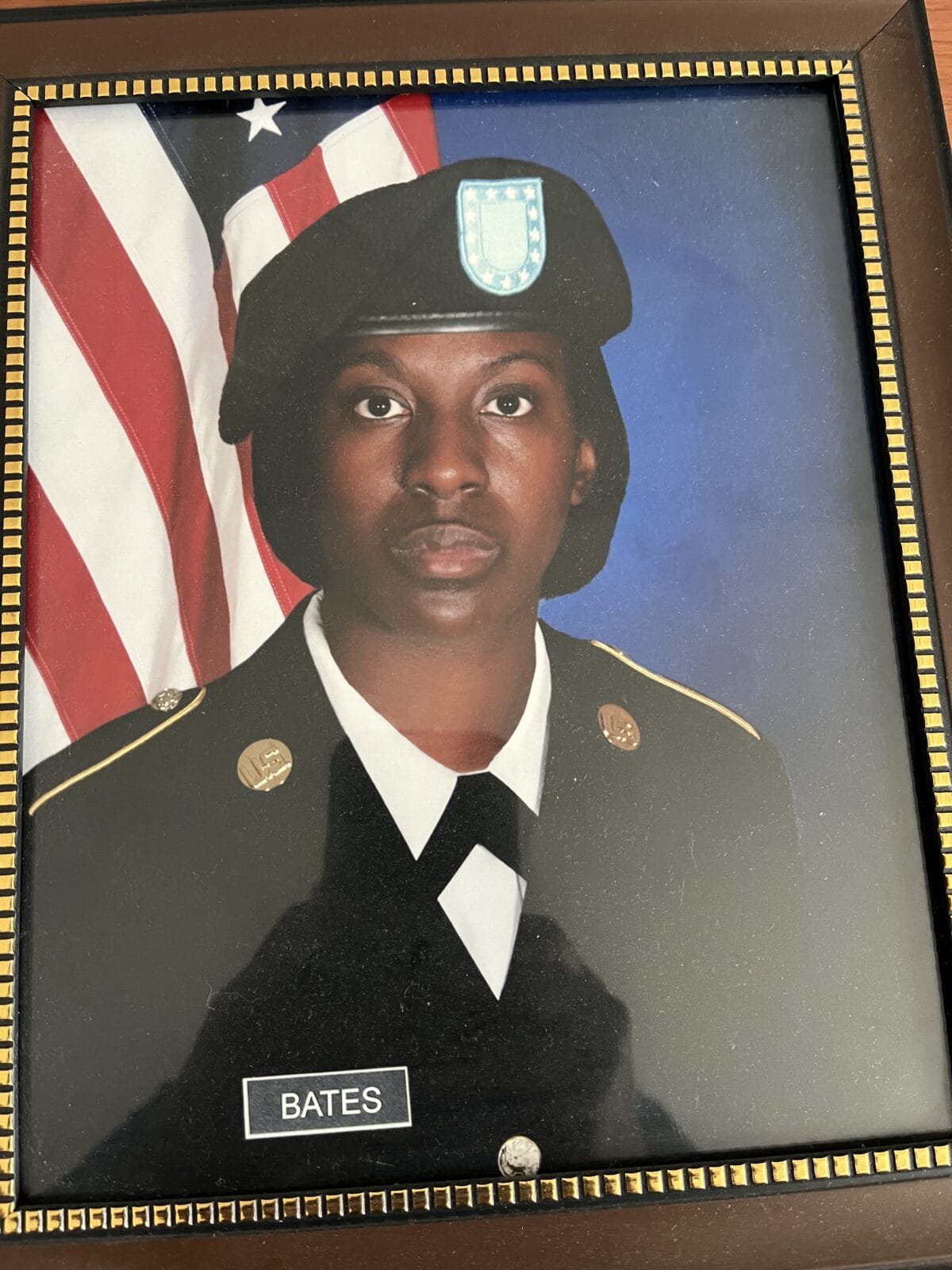
Warrior for Answers: Q&A with Taisha
Taisha’s Story, January 2025
As told to: Diego Colon
Diagnosis received: Post-traumatic stress disorder, Anxiety, Migraine, Neuropathy
Symptoms: Head pain, Noise and light sensitivity, Nausea, Vomiting, Hyperventilation, Vertigo
With 4.5 unforgettable years of military service, U.S. Army National Guard veteran, Taisha, has lived with migraine disease for over 10 years. Although her symptoms were present while on active duty, her condition began to take a toll on her life even more so when returning to civilian life. Now, as a former Sergeant and since becoming familiar with the U.S. Department of Veterans Affairs system (VA), Taisha has aimed to take a holistic approach in managing her migraine disease. Here, she retraces how she navigated the start of her migraine attacks and its challenges, and the process of seeking care within the VA healthcare system.

Q: Can you tell us about your military background? Are your migraine attacks service-related?
So, my migraines are service-related. It was kind of a trigger. I do have post-traumatic stress disorder (PTSD) from a traumatic event that has sustained, well endured, while I was enlisted. I wasn’t even assigned to my unit just yet; I was still in the U.S. Army Training and Doctrine Command (TRADOC).
Q: When were you diagnosed with migraine?
I was still [on] active duty when I was first diagnosed. It was actually 2011, so it’s been more than 10 years. It was right after I came back home. It had just gotten worse when I took on that job around 2013 – 2014 because I was constantly in front of a computer. The condition worsened around that time.
Q: What symptoms did you experience that indicated you were having a migraine attack?
I know my migraines are brought on by my anxiety attacks… The first thing to go is literally my mind. Everything around me… the lights are getting bright; the noise is loud. Sometimes it’s to the point where I have to lie down underneath my blanket and lie on my side just in case I have to throw up because of the intensity of it all. That’s when I start hyperventilating… That’s when I have to go to the hospital or the local VA to help get rid of the migraines, because it can get that bad… They had to shoot [infuse] me with tramadol or morphine* at one point, because it [the migraine] is that abrasive.
Q: When you first started developing migraine symptoms, what were some things that led you to the doctor? What made you think, ‘This might be something more?’
I think when it started to affect my everyday life. It started, for example, as soon as I came back from the Army, I was looking for a job, of course. Then the transition from feeling like you’re the big man on campus… The transitional phase was just hard… we go from feeling like hires of honor, just being able to serve your country, to being just like everyone else. You’re trying to figure out your placement. That’s where my migraine started because it was more of that ugly thing called “imposter syndrome” [that] was triggering my PTSD [and] was triggering my migraines.
I was placed on Family Medical Leave Act (FMLA), and you do not get paid. So, as a single mother, that was another trigger. It was just me. I have a child to take care of. At the time he was four, I’m trying to go to grad school. So, it’s just like, ‘Oh my gosh. This is a lot for me to take on,’ and the migraines were just so bad. I think every week, I was out of the office. Every week, because I couldn’t take the lights, and on top of the blue lights, it was just brightly lit in the office because it didn’t have windows, so all the lights were on… It was just a lot.
Q: Can you tell us more about trying to exist in your workplace with migraine disease? What’s that balance like for you?
Now, it has gotten better just because, you know, a pandemic changed that. So now, no one has a typical work environment. We’re either hybrid or 100% remote. On those days that I am working remotely, I am able to take breaks… from the screen, things that I know trigger them and [from] being at my laptop all day. I just try to take breaks here and there.
When I’m at school, I have coffee, I have things that cause triggers, like chocolate snack foods, because, you know, I work at a university. I have all of those things in my face… When I’m on campus, I’m able to take a quick break in my car, because I have blackout tint, and I relax for a couple of minutes and listen to some Lo-Fi music just to help center myself. I do have ginger candy, because ginger candy does work with my nauseating feeling that I feel with migraines, or I try to have some type of minty gum to close up the vessel a little bit. I just try to do a less abrasive medicinal approach.
Q: What does your migraine treatment/care consist of?
Being a veteran with PTSD, my treatment mechanisms are serotonin-based, or sertraline (zoloft), and a second one, I can’t think of the other antidepressant. It’s basically a cocktail [that] incorporates [my] neuropathy. The medicine that I’m being treated for neuropathy also has [been effective in treating] my migraines. But being a person who works, it makes me sleepy, and I don’t like it, so I’m trying to steer towards a more holistic approach…
For example, I just drank, it’s not flattering on the taste, but I feel better with [it]. It’s warm water, lemon, cinnamon, turmeric, and ginger… there’s a lot of anti-inflammatory benefits associated with all types of herbs and spices that I just mentioned. So, that’s my whole thing and try[ing] more mindful-based techniques…
I love the VA for what it stands for. With my situation, I have one kidney, so it’s certain medicines that I cannot take anyway... I’m doing my own personal research on how I can fight migraines without the abrasive techniques, or shooting [injection] onabotulinumtoxinA in my head, or taking all these pills.
Q: What do you think ‘you’ today, would say to ‘you’ back then about your migraine journey?
It gets better. Stop looking for the quick approach when it comes to… medicines, because, of course, it helps the onset of the migraines, but also the side caveat, [what] people don’t want to talk about sometimes [is] some migraine medicines give us a sedated feeling which we like… the altered state of being, or your heightened state of being, so don’t seek that.
Just take the time and do the research. There are more organizations like the National Headache Foundation, promoting more headache and migraine wellness now. Ten years ago, I never would have thought I would be on a conversation right now talking about ‘How can I alleviate migraines?’
Q: What did you say to your doctors with the VA that led to a turning point where they concluded, ‘This is something different. This is migraine disease’?
It’s more so when I had to be seen by a community care neurologist. At the time, I guess the situation was beyond the area of expertise. The amount of care depends on where you live demographically. I resided at the time in Kentucky, so it was kind of behind the curve a little bit on the different services that are offered to veterans. I had to see the closest [VA] hospital... Plus, I know I’m not the only veteran within central Kentucky. The waiting list was so long, and I needed immediate answers, because I was literally getting written up for work for missing so many days prior to my probationary period. I was like, ‘Hey, I need immediate action. Can I just see someone on-site? Sign appropriate paperwork to release my records to the VA.’
Q: The doctors scheduled you to see a neurologist shortly after that?
Surely, I did my own research on it… Or [searching for] the best neurologists within my address, within this amount of radius. Or sometimes I do look at social demographic factors too, with my ethnicity and me being a woman, I am part of a marginalized community. I don’t want anyone to feel as though, ‘Oh, there’s nothing wrong with you.’ No, there is something wrong with me. It’s unnatural for me [that] every time I have a headache, I feel like I have to throw up, or my vertigo is off, or like it’s completely debilitating.
Q: Did you come up against a significant amount of, not just the stigma around marginalization, but also the stigma around pain?
Of course, it was both! It was definitely both. Especially being a veteran, that’s not something you want to admit, that you’re in pain… As a veteran, you don’t want to admit that you feel weak. It’s not in our vocabulary.
It was slowly but surely getting to the point of, ‘Hey, I can’t mask this pain anymore. I have to let someone know, because it’s starting to affect my work performance, even with the military.’
Q: What is something you would want to ask from Congress about advocacy for migraine disease?
Stop minimizing it. Actually, take it seriously. Have initiatives that support it, just potentially, have some type of training on it, because it’s really a debilitating thing out there. There has been some research showing that migraine has been linked to debilitating pain diseases. If you have a debilitating pain disease, there’s nothing that can stop the pain, which causes a rise in suicide, because the pain is so unbearable. It’s not just a headache...

Disclaimer: The use of opioids is not recommended for the treatment of headache disorders or migraine disease. Evidence suggests they may be ineffective and carry significant risks of medication overuse headache and dependance. (American Headache Society, 2019)
If you are experiencing headache or migraine attacks, consult a healthcare provider to work closely with a migraine specialist to develop a personalized treatment plan.
